Did you know that women are more likely to develop Alzheimer’s disease than men? In fact, about two-thirds of Alzheimer’s cases in the U.S. affect women. One key factor that might help explain this disparity is the connection between sleep disruptions, Alzheimer’s disease, and sex differences. As a recent study shows, it’s becoming clear that sleep problems, especially during and after menopause, may play a significant role in women’s increased risk for Alzheimer’s.
The role of sleep in Alzheimer’s disease
Sleep is essential for our health, especially for our brains. During sleep, the brain clears out waste products, including proteins linked to Alzheimer’s disease, like amyloid-beta. Poor sleep, particularly in middle age, can increase the risk of Alzheimer’s by interfering with this cleanup process. Sleep issues—such as insomnia, disrupted deep sleep, and sleep apnea—are common among people with Alzheimer’s. Moreover, those issues often worsen as the disease progresses.
However, what’s particularly interesting is the connection between sleep, Alzheimer’s disease, and sex differences, as described in Sex and Sleep Disruption as Contributing Factors in Alzheimer’s Disease, published earlier this year in the Journal of Alzheimer’s Disease by a team of researchers at the University of Kentucky led by M. Paul Murphy, MA, PhD.
Women have more sleep disturbances than men, especially when experiencing menopausal symptoms. Studies show that women are more likely than men to report poor sleep quality, including difficulty falling and staying asleep. This could be related to the fluctuation and eventual decline of hormones like estrogen and progesterone, which help regulate sleep, and an increase in follicle-stimulating hormone (FSH). This, in turn, seems to increase women’s risk of developing Alzheimer’s disease.
“The association during aging of increased sleep disruption and sleep disorders, dramatic hormonal changes during and after menopause, and increased Alzheimer’s disease pathology may be interacting and contributing factors that lead to the increased number of women living with Alzheimer’s disease.”
Johnson CE, Duncan MJ, Murphy MP. Sex and Sleep Disruption as Contributing Factors in Alzheimer’s Disease. J Alzheimers Dis. 2024;97(1):31-74. doi:10.3233/JAD-230527
Hormones, sleep, and brain health
Menopause, with its dramatic hormonal changes, has been strongly linked to sleep disruptions and increased Alzheimer’s disease pathology. The hormonal shifts during menopause don’t just affect sleep—they also have a profound impact on brain health. Estrogen, for instance, plays a protective role in the brain by supporting memory, cognitive function, and sleep quality. As estrogen levels drop, the risk of developing Alzheimer’s disease increases. What’s more, researchers have linked the rise in FSH during menopause to sleep disturbances and Alzheimer’s disease progression.
In addition to estrogen and FSH, other hormones like progesterone and luteinizing hormone also influence sleep and brain health. Progesterone, for example, promotes deep, restorative sleep. When these hormone levels drop, women may experience more fragmented sleep. This can further contribute to the build-up of harmful proteins associated with Alzheimer’s disease.
Research shows that women have more amyloid beta (Aβ) and tau build-up in the brain than men, especially after menopause. These proteins are hallmarks of Alzheimer’s.
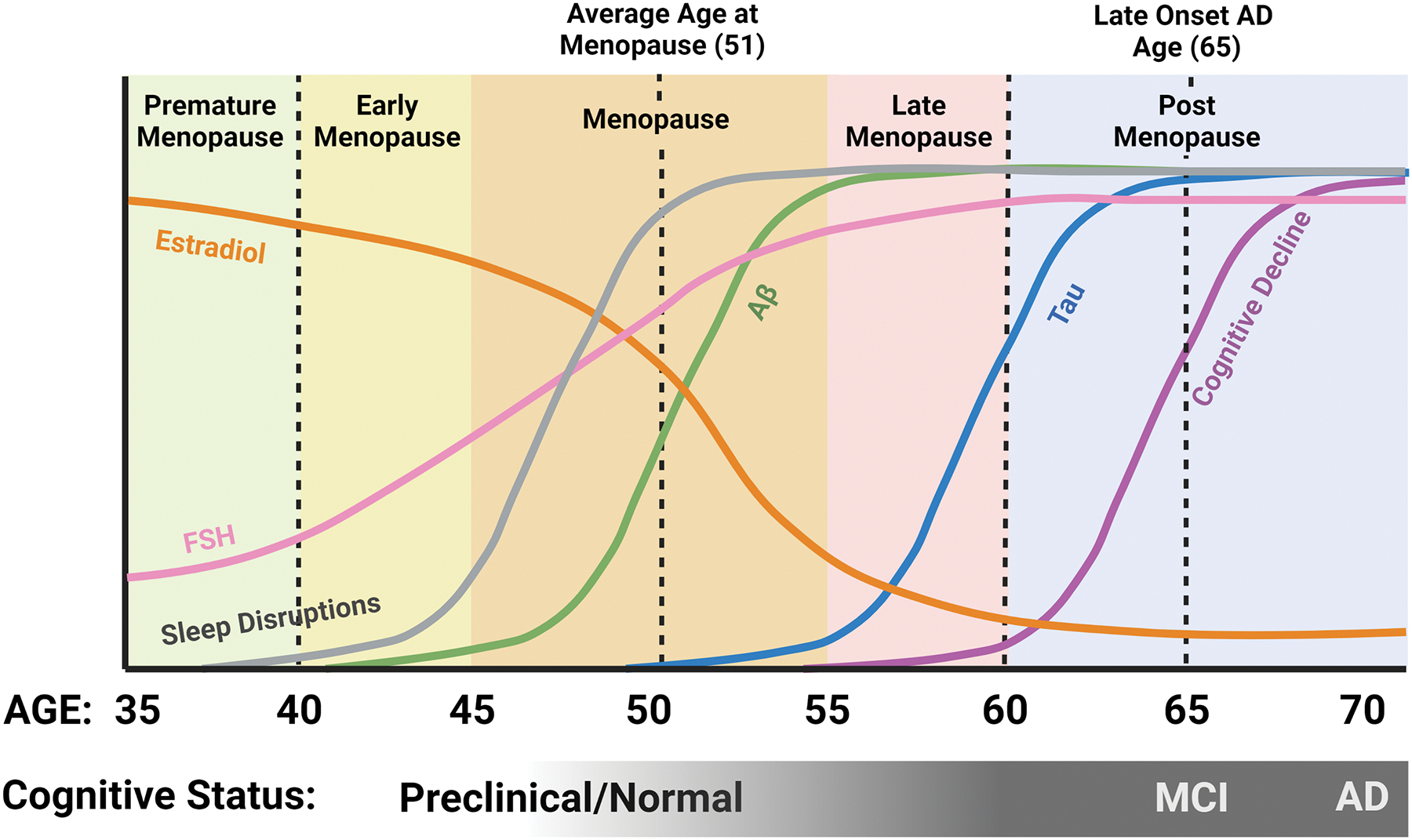
Relationship between sleep, hormones, and AD pathology in women
Estradiol levels begin to decline pre-menopause, while FSH levels begin to rise. Sleep disruptions become prominent during the menopausal transition, about the time when Aβ levels in the brain begin to increase. This is followed later by an increase in tau. Although some cognitive issues may start in late menopause, the majority of AD-related cognitive decline occurs post-menopausal. Created by Carrie E. Johnson.
Sleep disorders and Alzheimer’s risk
Sleep disorders affect millions of people worldwide, but they are especially prevalent in women. Insomnia, for instance, affects more women than men and researchers have linked it to cognitive decline and brain atrophy. Restless legs syndrome (RLS), another common sleep disorder, is also more frequent in women. RLS may worsen with age, contributing to cognitive problems and an increased risk of Alzheimer’s.
Additionally, women are more likely to experience obstructive sleep apnea (OSA) after menopause. OSA, a condition where breathing repeatedly stops and starts during sleep, is a risk factor for Alzheimer’s, as it is linked to increased amyloid and tau levels.
Men also experience sleep issues as they age, but women, particularly those going through menopause, appear to be hit harder. The connection between sleep, Alzheimer’s disease, and sex differences is more than just hormonal; sleep disorders like insomnia, RLS, and OSA are all more common in women and researchers have linked them to cognitive decline and Alzheimer’s.
Sex and bias in medical research
Why hasn’t science made more progress in addressing the disproportionate impact of Alzheimer’s disease on women? Sex bias likely plays a role. Historically, most medical research has focused on male subjects due to the perceived complexity of fluctuating hormones in females. These hormonal changes affect clinical outcomes and responses to therapies. As a result, women have often been underdiagnosed and inappropriately treated. Though women consume nearly 80% of prescription drugs in the U.S., doctors still prescribe dosages for them based on male physiology, increasing their risk of complications. It wasn’t until 1993 that the U.S. National Institutes of Health (NIH) required the inclusion of women in research. Only in 2014 did the NIH mandate considering sex as a biological variable.
Progress has been slow. By 2019, women made up about half of NIH-funded clinical research participants, but fields like neuroscience still lag. A 2020 study found that just 52% of articles in top neuroscience journals included female subjects. In Alzheimer’s research, only one-third of participants are women. The NIH only allocates 12% of its budget for the disease to female-focused studies.
Moving forward
As we continue to explore the links between sleep, Alzheimer’s disease, and sex differences, it’s becoming clear that understanding these interactions is crucial for developing more effective treatments. With more research, experts might be able to design therapies that target the specific sleep challenges women face as they age, especially during and after menopause. By addressing these sleep issues, we could potentially reduce the risk of Alzheimer’s disease and improve the quality of life for millions of women.
See a summary of the Parsemus Foundation’s Alzheimer’s Disease Prevention Project here. See our previous blog posts on the topic here.
See a summary of our Hormones for Menopause project here. See our previous blog posts on the topic here.