Recent research has spotlighted melatonin as a potential ally in the fight against Alzheimer’s disease (AD). Scientists from Zhejiang University and Uppsala University published a comprehensive review in the journal Molecular Psychiatry in August 2024, exploring how this natural hormone might protect brain health.
“The evidence from both animal and human studies suggests that melatonin has significant potential as a therapeutic agent for improving cognitive function and mitigating cognitive impairments associated with AD,” the scientists wrote in the review.
Understanding Alzheimer’s disease
Alzheimer’s disease is the most common cause of dementia, affecting more than 50 million people worldwide. Its hallmark features include the buildup of amyloid-beta plaques and neurofibrillary tangles, which damage brain cells. Scientists are increasingly focusing on how modifiable factors, like sleep, influence AD development. Sleep disorders (such as insomnia and obstructive sleep apnea) have been linked to an increased risk of Alzheimer’s, possibly because sleep helps clear harmful brain waste products. And people with Alzheimer’s disease may develop poor sleep processes.
Melatonin’s role in brain health
Melatonin, a hormone primarily produced in the pineal gland of the brain at night, regulates sleep-wake cycles and is a potent antioxidant. Research suggests that in addition to improving brain waste clearance, melatonin can:
- Reduce amyloid-beta production and modulate the tau protein.
- Reduce oxidative stress in the central nervous system.
- Influence circadian processes in brain cells.
- Support healthy insulin signaling, which influences Alzheimer’s progression.
- Strengthen the blood-brain barrier, safeguarding the brain from harmful substances.
Dr. Christian Benedict, a sleep researcher at Uppsala University and an author of the review, highlighted these mechanisms in an interview published by the university. He explained that melatonin even boosts cognitive abilities.
“For older people with reduced body production of melatonin, supplements in tablet form may very well be a positive ingredient for good cognitive aging,” Dr. Benedict noted.
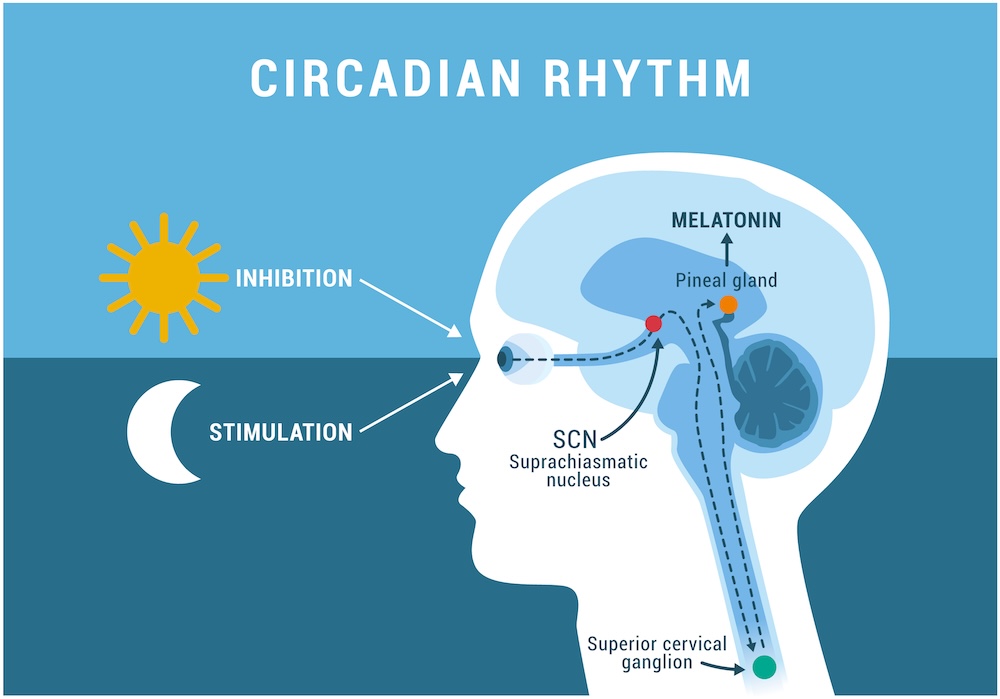
The circadian rhythm and sleep-wake cycle: how exposure to sunlight regulates melatonin secretion in the human brain and body processes
Key findings and limitations
Animal studies and early human trials show encouraging results. For instance, melatonin has been found to:
- Decrease the formation of amyloid-beta and tau tangles in lab settings.
- Improve cognitive scores in individuals with mild Alzheimer’s.
- Enhance sleep quality and reduce agitation in nursing home residents.
However, significant gaps remain. Most evidence comes from cell lines and animal models, and the long-term effects of melatonin in humans are not well understood. Concerns include potential side effects, such as disrupted insulin production or an increased risk of nighttime falls due to drowsiness.
What’s next for research on melatonin for Alzheimer’s disease?
The review emphasizes the need for rigorous clinical trials to determine the optimal dosage, timing, and formulation of melatonin for Alzheimer’s prevention or treatment. Innovative approaches, like intranasal melatonin delivery, could enhance its brain-targeting potential. The researchers recommend additional studies that compare melatonin use with brain pathology in older adults, which can be measured with PET scans, cerebrospinal fluid tests, and newer blood plasma biomarker analysis.
Supporting brain health naturally
While we await more definitive answers, experts suggest optimizing your body’s natural melatonin production:
- Maintain a consistent sleep schedule.
- Limit exposure to artificial light at night.
- Get plenty of natural light during the day.
- Avoid caffeine and alcohol close to bedtime.
These steps, combined with physical activity and a balanced diet, may promote overall brain health and reduce the risk of Alzheimer’s.
Conclusion
The evidence so far underscores the potential of melatonin as part of a broader strategy to combat Alzheimer’s disease. While it’s not a cure, its affordability, accessibility, and protective properties make it a compelling area for further research.
Read our web page on Alzheimer’s disease prevention, and see our other news articles on the topic.