Most research on Alzheimer’s disease (AD) involves new diagnostic or treatment methods. But did you know that being diagnosed with AD depends on where you live?
A large percentage of people in the United States with AD or dementia are undiagnosed. This could be due to various factors, such as patient concerns about stigma or local physician skills. Early diagnosis is critical, though, so patients can start treatment at an early stage of the disease when it’s more likely to be effective. Understanding the reasons for underdiagnosed disease is important so that healthcare providers can craft strategies to address the problem.
Different parts of the United States have different rates of Alzheimer’s diagnoses. Scientists from the University of Michigan sought to determine whether the regional variation in diagnosis was due to risk factors related to the specific population or the intensity of new cases diagnosed. As published in Alzheimer’s & Dementia, the researchers determined the diagnosis rate of AD and similar dementias across the United States using national Medicare claims data (see map).
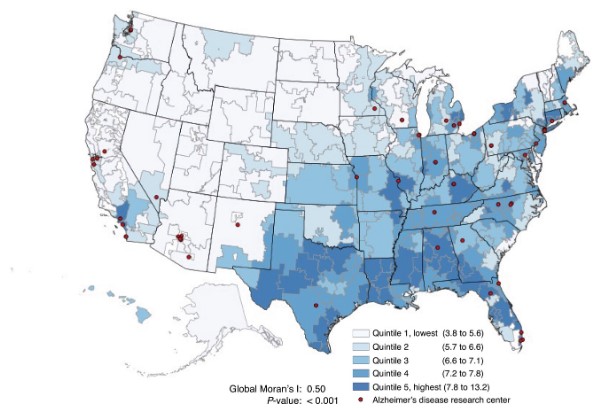
Geographic distribution of total older adults (≥66) diagnosed with AD or related dementias (no. per 100) in fee-for-service Medicare by U.S. hospital referral regions, 2019. From Bynum et al. 2024.
The Stroke Belt and Alzheimer’s diagnoses
More diagnoses of AD or related dementias occur in the Southeastern and the Midwestern United States. Prior studies characterized this region as the “Stroke Belt” due to the higher incidence of stroke in this region. Some researchers have indicated that contributors to the Stroke Belt may include a larger proportion of Blacks and residents with more stroke risk factors, higher prevalence of inflammation and infection, and lower socioeconomic status.
Earlier studies on regional variation in AD incidence did not evaluate underlying risk factors as well as the area’s “diagnostic intensity.” To fill this knowledge gap, the research team constructed a measure of the diagnostic intensity of AD by comparing the observed (actual) number of new cases to the expected number of cases for 2019. They adjusted the information in the map above to account for underlying sociodemographic and population dementia risk factors simultaneously, as well as diagnostic intensity for disease.
When considering all the factors, they still found geographic differences in the likelihood of being diagnosed, but the variation didn’t follow the “Stroke Belt” scenario (see map below). Instead, the number of new diagnoses varied across regions related to age, race/ethnicity, underlying dementia risk factors (such as obesity, diabetes, and smoking), and differences in how aggressively diagnoses across regions are sought out.
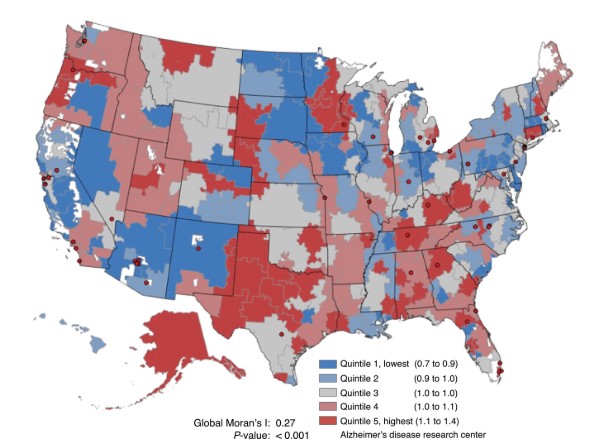
Geographic distribution of AD and related dementia diagnosis intensity by U.S. hospital referral regions among older adults (≥66) in fee-for-service Medicare, 2019. From Bynum et al. 2024.
Conclusion
The study concluded that “The implication of these results for individuals is that care in some health systems or areas may be more inclined toward recognition and diagnosis of [AD and related dementias]. And the differences across place are greatest for younger, Black, or Hispanic older adults.”
This evaluation can help to point researchers and clinicians toward improving local healthcare services to address lower-than-expected new diagnoses of AD and dementia. This is particularly important for minoritized racial or ethnic groups.
Read our web page on Alzheimer’s disease prevention, and see our other blog posts on the topic.



