Project Summary
Please note: This is an archived project that is not currently being updated.
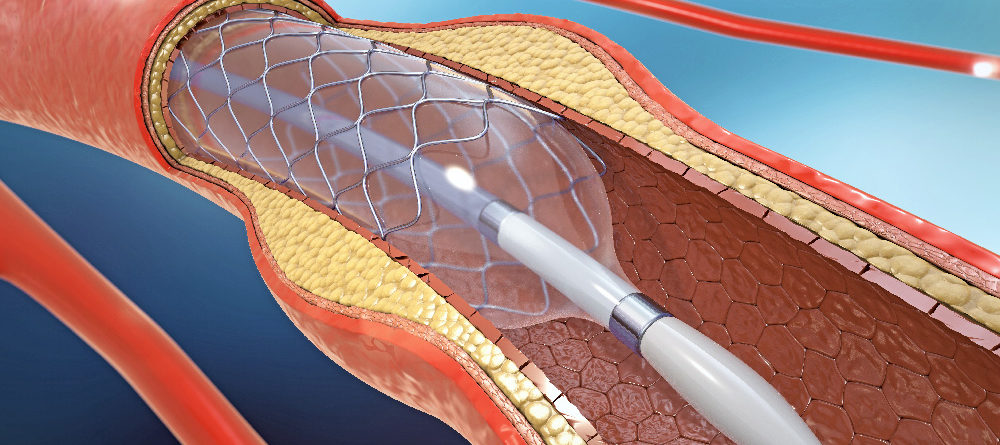
Angioplasty and stenting continue to be used in stable coronary artery disease (i.e. not in the middle of a heart attack), even though large randomized controlled trials have shown that they add no significant survival benefit. Angioplasty and stenting are exceedingly expensive and carry risks (including heart attack and stroke) to the patient. For more information on over-used medical treatments, see our page on Evidence-based Medicine.
Project Topics
Angioplasty and stenting may be overused
The COURAGE study reported in 2007 that angioplasty and inserting stents, or PCI (percutaneous coronary intervention), provided temporary relief from angina, but did not result in fewer deaths, myocardial infarction, or cardiovascular events than medication and lifestyle changes. The OAT clinical study indicated that for high-risk patients with total occlusion of the infarct-related artery, PCI conducted after the myocardial event did not reduce the risk of death, re-infarction, or heart failure.
The data were a shock to many cardiologists, who saw symptomatic relief in patients and have been performing angioplasties and inserting stents in a good-faith effort to help improve quality of life.
Despite this information and the changes to professional medical society guidelines, a 2011 study reported no decline in the use of PCI. A number of media outlets covered the news, raising awareness among the public and questioning the continued reliance on procedures that were not shown to be effective.
Surely by now — years after additional research and attention to the issue — the use of angioplasty and stenting should have decreased. But unfortunately that is not the case, and it may be a matter of money. Recent cutbacks on healthcare revenue are being blamed for the overuse of stents — doctors make much more money through the $30,000 stent procedure than by spending time with the patient discussing the alternative: medication and lifestyle changes. In fact, in 2013 the Joint Commission and the American Medical Association Physician Consortium for Performance Improvement cited elective PCI on patients with stable coronary artery disease as one of the most overused medical procedures. And in 2017, a comprehensive investigation about overused medical procedures in The Atlantic pointed to the use of angiogram and stents as procedures that continue to be prescribed by physicians despite studies showing little benefit — and sometimes harm.
Some patients and doctors may also think that PCI helps to solve the “plumbing” problem of a blocked artery, but inflammation is a contributing factor and most ruptures occur at mild lesions. Misconceptions about the relationship between cardiovascular disease and narrowed arteries — with most patients erroneously expecting that a stent will reduce the chance of a future heart attack — may also be at the root of the overuse of the procedure. As many as a million patients in the U.S. may have been given stents they don’t need in the last decade. Unnecessary stents cost upwards of $2.4 billion a year to our healthcare system.
To raise awareness of this issue, the Parsemus Foundation has supported the publication of articles analyzing and discussing peer-reviewed studies on appropriate and inappropriate use of angioplasty and stenting. Our goal is to prevent patients and loved ones from facing unnecessary risks and in some cases debilitating medical expenses, without a clear expected benefit. Most patients undergo angioplasty because they believe it may save their life; if that is not the case, then they (and their doctors) deserve to know the full picture.
Media Coverage:
2011
- OAT Trial Had Little Impact on Clinical Practice, Forbes
- Guidelines Don’t Curb Unnecessary Treatment for Heart Attack Patients, Bloomberg
- Adherence to Angioplasty/Stent Guidelines Lacking: Study, U.S. News & World Report
- Heart Stents Still Overused, Despite Guidelines: Study, Huffington Post
2013
- Heart stents still overused, experts say, New York Times
- Deaths Linked to Cardiac Stents Rise as Overuse Seen, Bloomberg
- The Good, the Bad and the Ugly: Stents in the News, Forbes
Additional Resources
A few relevant background studies:
- Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GB, Weintraub WS; COURAGE Trial Research Group. Optimal Medical Therapy with or without PCI for Stable Coronary Disease. (2007) N Engl J Med. 356:1503-1516. Free full text
CONCLUSIONS: As an initial management strategy in patients with stable coronary artery disease, PCI did not reduce the risk of death, myocardial infarction, or other major cardiovascular events when added to optimal medical therapy. - Lin GA, Dudley RA, Redberg RF.(2007). Cardiologists’ use of percutaneous coronary interventions for stable coronary artery disease. Arch Intern Med.167(15):1604-9.
CONCLUSIONS: The widespread application of PCI in stable coronary artery disease for indications unsupported by evidence may reflect discordance between cardiologists’ clinical knowledge and their beliefs about the benefits of PCI. Nonclinical factors appear to have substantial influence on physician decision making. Future studies should focus on the development of methods to help providers more fully incorporate clinical evidence into their medical decision making. - Lin GA, Dudley RA, Redberg RF (2008). Why physicians favor use of percutaneous coronary intervention to medical therapy: a focus group study. J Gen Intern Med.23(9):1458-63. Free full text
CONCLUSIONS: The widespread use of PCI in patients with stable coronary artery disease–despite evidence of little benefit in outcomes over medical therapy–may in part be due to psychological and emotional factors leading to a cascade effect wherein testing leads inevitably to PCI. Determining how to help physicians better incorporate evidence-based medicine into decision-making has important implications for patient outcomes and the optimal use of new technologies. - Lin GA, Dudley RA, Lucas FL, Malenka DJ, Vittinghoff E, Redberg RF. (2008) Frequency of stress testing to document ischemia prior to elective percutaneous coronary intervention. JAMA. 300(15):1765-73. Free full text
CONCLUSIONS: The majority of Medicare patients with stable coronary artery disease do not have documentation of ischemia by noninvasive testing prior to elective PCI. - Siontis GC1, Tatsioni A, Katritsis DG, Ioannidis JP.(2009) Persistent reservations against contradicted percutaneous coronary intervention indications: citation content analysis. Am Heart J.157(4):695-701.
CONCLUSIONS: Despite strong randomized evidence, a fraction of the literature, mostly corresponded by interventional cardiologists, continues to raise reservations about recently contradicted indications of PCI.
- Last updated on January 30, 2023
Human Health News
Nanotechnology targets cancer through breast ducts
Breast cancer remains a significant health challenge worldwide. While advancements in treatment have improved survival rates, the search for more targeted and effective therapies continues. Nanotechnology-based intraductal drug delivery aims to revolutionize local treatment and prevention of breast cancer by delivering nanocarriers with therapeutic agents directly to the site of the disease.

Vision loss and dementia risk
A recent study found that up to 19% of dementia cases may be attributable to impaired vision. The study, published in JAMA Ophthalmology, showed that vision loss may have even more of an impact on the risk of dementia than previously thought. Hearing loss is also considered a modifiable risk factor for dementia, supporting the notion that sensory engagement is critical for brain health.

Blood tests predict cardiovascular disease
Cardiovascular disease is the leading cause of death worldwide. Heart attacks, strokes, and other heart-related conditions claim millions of lives each year — more than cancer. In the U.S., cardiovascular disease kills someone every 33 seconds, and is responsible for more than 20% of all deaths, according to the Centers for Disease Control. But what if a simple blood test could help predict heart disease decades in advance?
Nanotechnology targets cancer through breast ducts
Breast cancer remains a significant health challenge worldwide. While advancements in treatment have improved survival rates, the search for more targeted and effective therapies continues. Nanotechnology-based intraductal drug delivery aims to revolutionize local treatment and prevention of breast cancer by delivering nanocarriers with therapeutic agents directly to the site of the disease.

Vision loss and dementia risk
A recent study found that up to 19% of dementia cases may be attributable to impaired vision. The study, published in JAMA Ophthalmology, showed that vision loss may have even more of an impact on the risk of dementia than previously thought. Hearing loss is also considered a modifiable risk factor for dementia, supporting the notion that sensory engagement is critical for brain health.

Blood tests predict cardiovascular disease
Cardiovascular disease is the leading cause of death worldwide. Heart attacks, strokes, and other heart-related conditions claim millions of lives each year — more than cancer. In the U.S., cardiovascular disease kills someone every 33 seconds, and is responsible for more than 20% of all deaths, according to the Centers for Disease Control. But what if a simple blood test could help predict heart disease decades in advance?

Regional variation in Alzheimer’s and dementia diagnoses
Different parts of the United States have different rates of Alzheimer’s diagnoses. Scientists from the University of Michigan determined that regional variation was due to risk factors related to the specific population as well as the intensity of new cases diagnosed.