Please note: This is an archived project that is not currently being updated.
Anti-estrogen therapy, such as aromatase inhibitors, are the standard of treatment for estrogen receptor positive breast cancer. A study in a postmenopausal mouse model had a surprising result: better survival and quality of life from bioidentical hormones, not anti-hormones, after breast cancer. While this line of research has not been continued in humans, we provide details about the study and controversy surrounding the use of anti-estrogen therapy. If you are facing decisions about breast cancer treatment, find a clinician who is up to speed on the latest scientific information, open to alternatives, and ready to evaluate your specific history and needs.
PROJECT
Questioning Aromatase
Inhibitors
HUMAN HEALTH
PROJECT
Questioning Aromatase
Inhibitors
HUMAN HEALTH
Project summary
Other women’s health projects
What if hormones aren’t fuel for the fire after all?
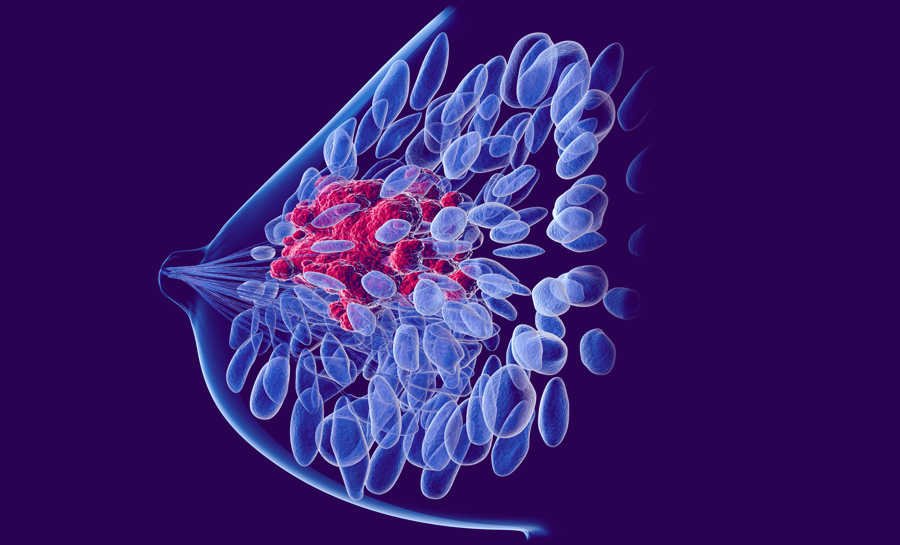
It’s no wonder that breast cancer ranks highest among women’s health concerns. Over 235,000 cases of breast cancer are diagnosed annually in the United States, with almost 40,000 deaths attributable to the disease. Although the leading cause of death in women is heart disease, cancer ranks second with breast, lung, and colorectal cancer being most common, according to the CDC.
Breast cancer is diagnosed more often in older, usually postmenopausal, women. Breast cancer treatments include anti-estrogen therapy, such as taking aromatase inhibitors, but the serious side effects lead many women to discontinue use. However, some research indicates that hormone replacement therapy using natural hormones may actually be a key component in the treatment of breast cancer.
Estrogen and anti-estrogen therapies
Estrogen is a steroid hormone that affects many areas of the body. Importantly, it influences bone and lipid metabolism, cardiovascular health, cognition, and sexual function. Postmenopausal estrogen replacement therapy is known to alleviate vasomotor symptoms like hot flashes, have a positive effect on the prevention of osteoporosis, and result in improved serum lipid profiles and reduced cardiovascular disease factors if started soon after menopause.
Despite the positive effects of hormone replacement therapy, it was reported to increase the incidence of breast cancer. In 2002, the Women’s Health Initiative (WHI) Study, which used synthetic estrogen and progesterone hormones, revealed a 24% increased risk for invasive breast cancer, with no major beneficial effects against cardiovascular disease, stroke, and thromboembolic diseases. While later findings refute these claims, the fear of breast cancer from hormone replacement therapy became widespread. Within three months, 63% of women stopped taking hormone replacement therapy.
Estrogen has also been targeted as the main hormone related to the growth of breast cancer, with most breast cancer treatments including anti-estrogen methods. For over 20 years, tamoxifen — a selective estrogen receptor modulator (SERM) — has been the favored treatment option. A newer class of medications called aromatase inhibitors has generally replaced tamoxifen for treatment of breast cancer in postmenopausal women.
After menopause, adrenal androgens are the main source of estrogen. Aromatase inhibitors act by preventing the aromatase enzyme from converting androgens into estrogens. Aromatase inhibitors such as anastrozole (Arimidex®), letrozole (Femara®) and exemestane (Aromasin®) come with serious side effects, though, including vasomotor symptoms, mood changes, loss of libido, vaginal dryness, joint and muscle pain, memory problems, and loss of bone density leading to hip fracture. In addition, in many patients resistance to both tamoxifen and aromatase inhibitors occurs over time, making them ineffective.
Clearly, an effective treatment for breast cancer — without all the serious side effects of aromatase inhibitors — is needed. Could hormone therapy be the answer?
Hormones and postmenopausal breast cancer
Despite the negative results of the WHI study, the relationship between hormones, breast cancer, and other health indicators is far from conclusive. Prior to the use of tamoxifen, estrogen therapy was actually the standard for the treatment of breast cancer (see Jordan and Ford, 2011 for historical review). Early comparisons of estrogen vs. tamoxifen treatment revealed that the synthetic estrogen DES provided as much protection as tamoxifen treatment (Peethambaram et al., 1999). In addition, more recent analyses of the Women’s Health Initiative data have shown that in hysterectomized women, estrogen replacement therapy alone actually seemed to decrease the incidence and mortality rate of breast cancer (Cheblowski and Anderson, 2012; Anderson et al., 2012).
Due to the confusion related to hormone therapy and breast cancer, meta-analyses of multiple studies have been conducted. In 2006, such an analysis indicated that hormone replacement therapy taken after breast cancer was related to a decreased risk of breast cancer deaths (Batur et al., 2006). Creasman (Creasman, 2005) reviewed studies on hormone replacement therapy after cancer, finding that case-control and cohort studies found no risk — or even less risk — of recurrence of breast cancer in women taking estrogen therapy. He concluded that hormone therapy has little if any risk to women who have had breast cancer.
If estrogen is related to breast cancer growth, how can it aid in the battle against breast cancer? Recall that breast cancer can become resistant to traditional anti-estrogen therapy. Acquired resistance occurs when the patient with an estrogen receptor-positive tumor initially responds to anti-estrogens but then suddenly the tumor begins to grow. Somewhat counter-intuitively, SERM-stimulated tumors may rapidly shrink in response to high-dose estradiol (a type of estrogen) treatment (see Ingle, 2002).
Synthetic vs. bio-identical hormones
The type of hormone given is important, as is the dose, combination of hormones, and duration of hormone treatment in relation to breast cancer. Synthetic hormones are often related to negative outcomes. But there is evidence that bio-identical hormones have been related to positive outcomes. Controversy about this topic has been hot. For example, a review article by Holtorf in 2009 indicated clear differences in activity and outcomes of bio-identical hormones vs. synthetic hormones, with bio-identical hormone treatment related to lower risks for breast cancer and cardiovascular disease. A separate review by Files and colleagues in 2011 concluded that even with some observational studies reporting decreased risk of breast cancer when using micronized progesterone and estrogen vs. synthetic compounds, more study is needed to confirm benefits of custom formulated bio-identical hormones due to variations in formulations, dosages, and delivery systems. Clearly there is a need for continued study of the impact of bio-identical vs. synthetic hormones.
Study on hormone replacement therapy provides insight
Review of the data indicates two conclusions:
- Hormone replacement therapy after breast cancer may not be counter-indicated
- The right hormone in the right dose given at the right time is critical
To ensure that the study of hormone replacement therapy and breast cancer continued, the Parsemus Foundation supported important pre-clinical studies of the use of bio-identical hormones – in various combinations and dosages – on breast cancer, cardiovascular health, bone health, and cognitive function. The study used a mouse model that mimicked postmenopausal breast cancer (the same model used for aromatase inhibitor approval studies). Groups of mice were treated with various amounts and combinations of bio-identical estradiol (a type of estrogen), progesterone, and testosterone as well as aromatase inhibitor in some cases. To understand the best combination for overall health, various factors were measured over time, including the impact on breast tumor growth, cholesterol and lipid profiles, bone specific alkaline phosphatase, memory, and activity.
A treatment of estrogen, progesterone, and testosterone resulted in increased cognition, physical activity, and cardiovascular and bone health in the mouse model. The maximal reduction in tumor growth was also found with this combination of hormones. Importantly, the tumor reduction was the same or better than treatment with aromatase inhibitor, and did not show a reduced anti-tumor effect over time that is common with the use of anti-estrogen therapy. Since aromatase inhibitors are the current standard of care, we also tested the impact of hormones used along with aromatase inhibitors. In this case, estradiol and progesterone improved the cardiac and bone health markers in the mice without promoting breast tumor growth. See Arumugam, Lissner and Lakshmanaswamy (2014) for the full text of the study.
This study offers insight into alternative treatment options for postmenopausal breast cancer patients using hormone therapy. The Parsemus Foundation urges more research in this area in order to find breast cancer treatments without significant side effects. However, we are not aware that natural hormone therapy for postmenopausal breast cancer has been studied more recently in humans. Most treatment plans still involve anti-estrogen therapy. But the type and timing of treatment is important. For example, ten years of aromatase inhibitor treatment instead of the standard five years may not provide much benefit when considering the side effects. This summary of a 2020 study questions the use of aromatase inhibitors for women with coronary artery disease due to long-term toxicity.
If you are facing difficult treatment decisions, be sure to find a clinician who is up to speed on the latest scientific information, open to alternatives, and ready to evaluate your specific history and needs in order to advise you on the best options.
Additional resources
A few relevant background studies:
- July, 2014 press release on the publication of research supported by the Parsemus Foundation.
- For a comprehensive review of research on the Women’s Health Initiative dataset, see this posting by Marcia Stefanick of Stanford University.
- Breast Cancer Choices has an overview of published literature showing the positive effects of hormone replacement therapy.
- Kronos Early Estrogen Prevention Study (KEEPS) studies the impact of estrogen therapy on cardiovascular disease.
- 2011 review article on the use of estrogen for prevention and treatment of breast cancer, published in the Journal of the National Cancer Institute.
- A meta-analysis comparing tamoxifen and aromatase inhibitors indicated that toxicity related to long term use of aromatase inhibitors is likely the reason for lower survival.